Senedd members scrutinised health chiefs about years-long delays to digital transformation of eye care, with some services still relying on paper records and fax machines.
Peter Fox, the newly elected chair of the Senedd's health committee, pressed witnesses about a lack of digital infrastructure "holding back" improvement in eye care services.
Digital Health and Care Wales (DHCW) was moved to level three on ministers' intervention framework in March due to concerns about its ability to effectively deliver major programmes.
Helen Thomas, DHCW's chief executive, said: "We know there are many opportunities that digital and data services can support...in terms of the challenges eye care services face."
"And we believe there is a way to go in terms of ensuring that they have the full digital infrastructure that is needed."
'Not delivered'
David Thomas, director of digital at the Cardiff and Vale health board, said an electronic patient record system has been deployed in all ophthalmology sub-specialties in his health board area.
But when asked about progress on digital stalling elsewhere, Ms Thomas told the committee DHCW hopes to complete a full national rollout after a current contract ends in early 2027.
The digital eye care programme began in January 2020, with £8.5m allocated by ministers.
A press release published in March 2021 said: "The project, being led by Cardiff and Vale university health board, has already commenced rollout across Wales."
Sam Hall, director of primary digital services at DHCW, said an electronic referral system was part of the original programme "but hasn't yet been delivered".
'Missed deadlines'
Former health minister Lesley Griffiths pointed out that the OpenEyes digital patient records project had an agreed deadline to be rolled out by March 2023.
"But this didn't happen," said the Labour MS for Wrexham. "So, I wonder if you could explain why it didn't happen and what the current status is please."
Mr Thomas pointed to the impact of the pandemic during the meeting on Wednesday.
Warning of problems getting people "on the same page", he said: "In hindsight, in terms of lessons learned, the engagement could have worked a lot better with other health boards."
He said OpenEyes is live in Cardiff and Vale, and one service at Cwm Taf Morgannwg, with plans to roll out the patient record system to all ophthalmology services within ten months.
Mr Thomas told the committee that Welsh Government funding covered capital spending, leaving health boards to meet the everyday costs such as employing more staff.
'Financial constraints'
He explained additional funding has been requested, given wider financial constraints, to cover local implementation costs of around £50,000 for each health board,
"We do now have the buy-in from health boards to proceed," he said. "But we need to recognise that there was a period where things didn't progress as they should."
Emma Cooke, an executive director at Cardiff and Vale, added: "We weren't demonstrating its value to the rest of Wales...that's the big thing I think we should have picked up quicker."
Michael Stechman – clinical director for ophthalmology at Cardiff and Vale, and a consultant general surgeon – warned of a Wales-wide shortage of ophthalmologists.
He also raised concerns about the centralisation of services creating challenges – with major trauma, neurosurgery and vascular surgery all "competing" for theatre space.
'Life changing'
Turning to the Betsi Cadwaladr university health board, Mr Fox pointed out that about 40,000 patients in North Wales were waiting for ophthalmology outpatient appointments.
Carol Shillabeer, chief executive of Betsi Cadwaladr, replied: "It's probably fair to say the health board has not made as much progress over the past four-five years as other areas."
"It's something for us to learn from."
Ms Shillabeer, who was appointed in 2023, outlined a focus on community ophthalmology services to free up capacity for secondary care teams to see the highest-risk patients.
Pressed about underreporting of incidents, the chief executive emphasised the importance of transparency and candour due to potentially "life-changing" levels of patient harm.


 Swapping date night for drysuits at Barry Dock RNLI
Swapping date night for drysuits at Barry Dock RNLI
 13,900 French Rugby Fans fly into Cardiff Airport ahead of Six Nations Fixture
13,900 French Rugby Fans fly into Cardiff Airport ahead of Six Nations Fixture
 Vale Councillor blasts school funding in the county
Vale Councillor blasts school funding in the county
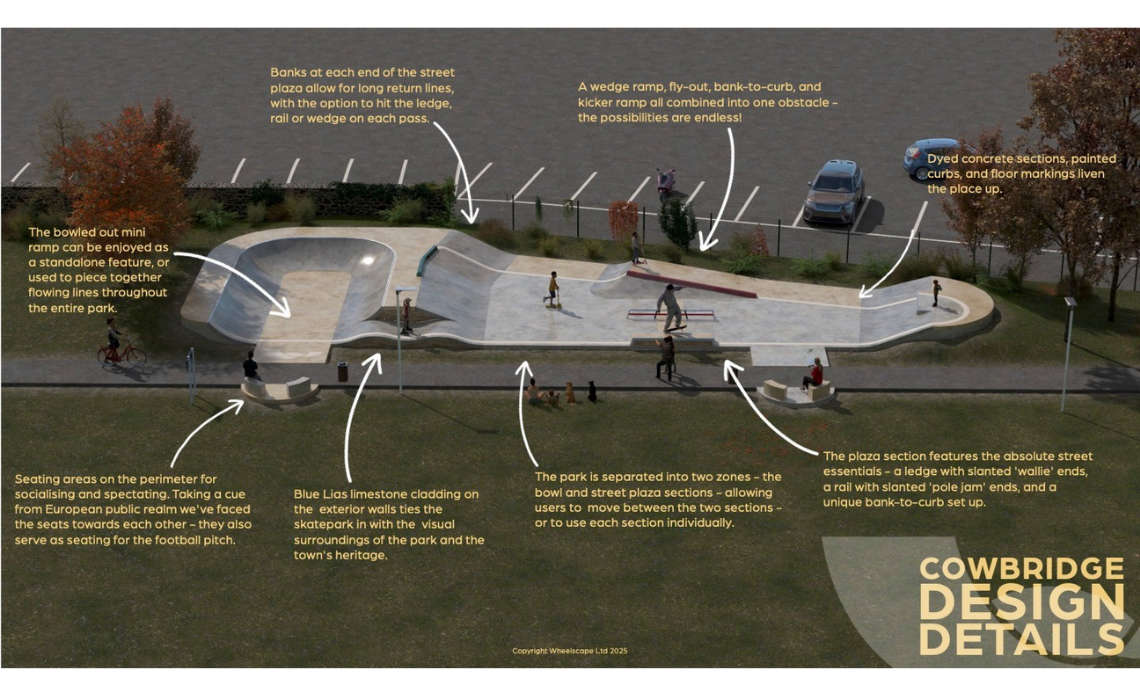 Bear Field Skate Park set for major upgrade as part of new Placemaking Plans
Bear Field Skate Park set for major upgrade as part of new Placemaking Plans
 New apprenticeship courses in construction to be introduced in Wales
New apprenticeship courses in construction to be introduced in Wales
 Former Penarth Bank could become a cafe
Former Penarth Bank could become a cafe
 New poll shows majority of Welsh voters lack voting confidence ahead of Senedd Election
New poll shows majority of Welsh voters lack voting confidence ahead of Senedd Election
 Construction hub secured for rail upgrades
Construction hub secured for rail upgrades
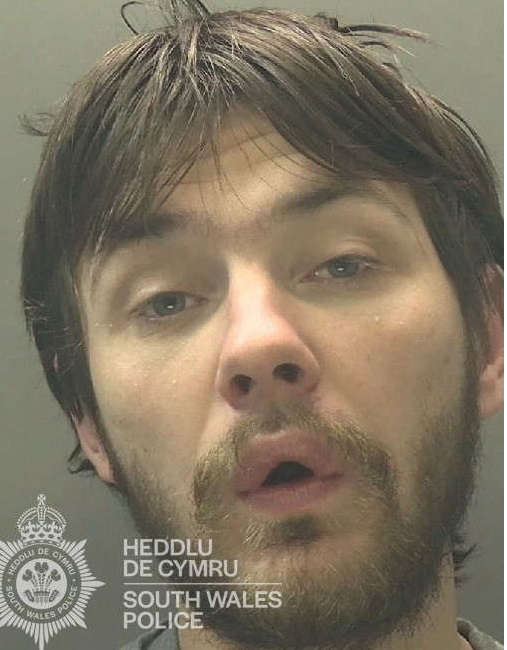 Prolific thief banned from Holton Road
Prolific thief banned from Holton Road
 Cowbridge: plans for more holiday lodges
Cowbridge: plans for more holiday lodges
 Man dies suddenly in Romilly Park
Man dies suddenly in Romilly Park
 Cash boost for Sully Primary School
Cash boost for Sully Primary School
 Speed limits reduced despite objections
Speed limits reduced despite objections
 Concern over imported chicken in school meals
Concern over imported chicken in school meals
 A48 closed after three-vehicle collision
A48 closed after three-vehicle collision
 Rhys unveils red bench 'in living memory'
Rhys unveils red bench 'in living memory'
 Barry: plans lodged for 70-home development
Barry: plans lodged for 70-home development